10 Things to Know About Male Infertility
Medically Reviewed by Dr. Kevin J Campbell, MD, a fellow in Male Reproductive Medicine and Surgery with Dr. Larry Lipshutlz, Professor of Urology, both at Bayor College of Medicine in Houston, TX.
On your path through fertility care, it’s easy to forget that men represent half the equation. Between monitoring ovulatoin, hormone injections, and the biological clock, most of the attention (and burden) is often put on women. On the other hand, testing for male infertility is often simple, low cost, and non-invasive. More importantly, 50% of infertility issues may be attributable to a male factor, soit’s vital to know as much information as you can about any potential issues.
To help you get started, we created an easy to understand guide to male infertility causes and treatment options for couples trying to conceive.
1. Back to Basics: How Babies are Made
Sperm are created from primordial germ cells in the testes. Around 300 million sperm mix with nutritive fluid from the prostate gland to form the ejaculate. On the female side, women ovulate once per month, sending an egg down into the uterus. Having sex anytime within the five days before ovulation may lead to a pregnancy if the sperm is able to fertilize the egg. After conception, the combination of the sperm and egg leads to embryogenesis (the first stages of new life).
2. Infertility Impacts 15% of All Couples
If you’re facing infertility issues, you’re certainly not alone. Infertility is defined as the inability to conceive a child within one year of unprotected sexual intercourse. Conversations around pregnancy often still revolve around female partners, but studies have shown that in 50% of cases, men play a significant role in the couple’s infertility. Another way of looking at this is that up to 7% of men may suffer from infertility. Illness, injury, age, chronic health problems, lifestyle choices, and other factors can contribute to male infertility. Worldwide, overall fertility rates have dropped about 1% per year between 1960 and 2018 for a variety of reasons–rising obesity, increasing cancer rates, chemical exposure, waiting longer to have children, and other changing lifestyle behaviors.
3. Common Causes of Male Infertility
Male fertility depends upon the ability to produce healthy sperm, maintain an erection, and ejaculate. Problems can arise with these functions due to hormonal imbalances, genetic disorders, or blockages. Possible causes include but are not limited to:
A few causes are:
- Varicocele (enlarged veins in the testicles)
- Undescended testicle
- Infection in the testicle or prostate
- Chemotherapy for cancer
- Anabolic Steroids
- Genetic Abnormalities
- Endocrine Abnormalities
- Ejaculatory Dysfunction
4. Factors that Increase Risk of Male Infertility
A number of risk factors are linked to male infertility, including:
- Aging
- Smoking tobacco or marijuana
- Drinking alcohol excessively
- Being overweight
- Exposure to environmental toxins
- Having past or present infections
- Overheating the testicles
- Having medical conditions, including tumors and chronic illnesses
- Taking medication or undergoing medical treatment such as radiation for cancer
- Testosterone therapy
In some of these cases, changing your lifestyle habits can improve your chances of conceiving a child.
5. Unexplained Infertility
Unexplained infertility affects 20-35% of all infertile couples. A diagnosis of unexplained infertility means that all fertility tests look normal for a couple, however, they are still unable to conceive without knowing why. Before getting to this point, a doctor will most likely have done a semen analysis for the male partner as well as a full assessment of ovulation and the fallopian tubes for the female partner. To be clear, abnormalities are still likely to be present in cases of unexplained infertility, but they are not detectable by current diagnostic methods.
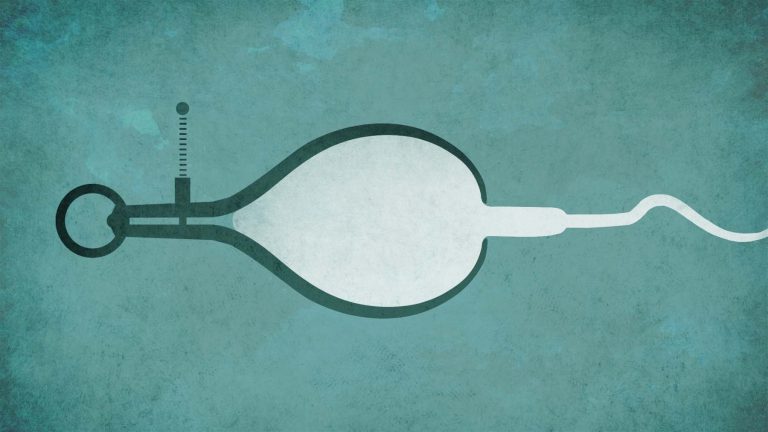
6. The Semen Analysis Test
The semen analysis is a fundamental lab test for testing infertility that assesses several parameters, including the number of sperm in a given sample, the motility of those sperm (can they move properly?), and the morphology (do they look normal?). This test also typically looks for signs of inflammation or infection (i.e., so-called “round cells” in the semen sample, which must then be differentiated from sperm germ cells). Although the semen analysis is a reasonable first test for assessing the male, it does not provide an overall evaluation of the fertility of the man. In other words, just because your semen parameters are normal doesn’t necessarily mean you’re fertile. Remember, a large proportion of infertile men are diagnosed with unexplained infertility.
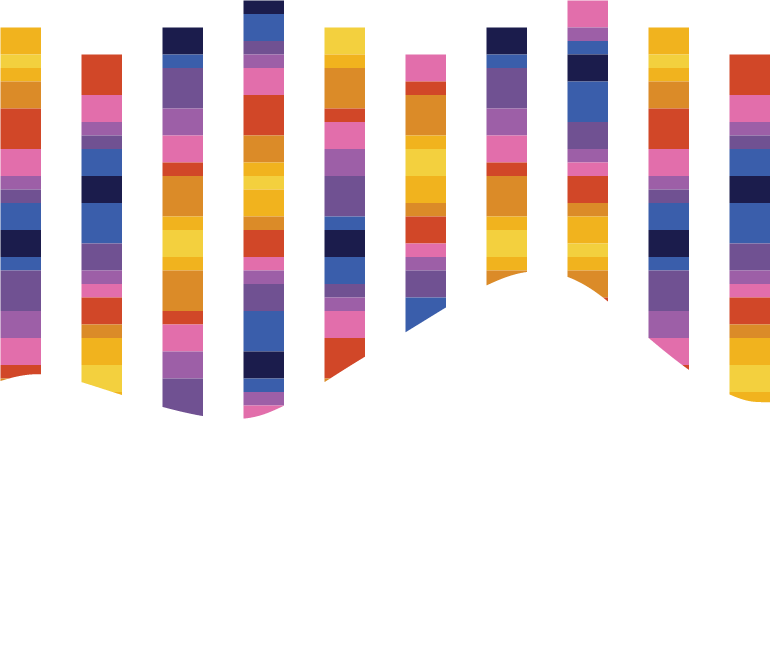
7. DNA Fragmentation Testing
DNA fragmentation is the separation or breaking of DNA strands into pieces. If a doctor suspects DNA fragmentation might be causing infertility, they can order a test to identify what percent of the DNA in a man’s sperm is fragmented. Common DNA fragmentation tests include the Tunel assay, Comet assay, or the Sperm Chromatin Structure Assay test.
8. Advancements in Testing for Male Infertility
Advances in diagnosing male infertility have been very limited over the last several decades. In fact, DNA fragmentation is considered one of the more recent advancements, but was discovered in 1980.
Path Fertility is raising the standard of male reproductive health by diving even deeper into the DNA and epigenetic profile of sperm. Our test, Path SpermQT looks at epigenetic patterns within sperm that specifically have to do with the ability to conceive. The test gives a result of Poor, Average, or Excellent sperm quality based on those epigenetic patterns. This result, combined with the information obtained from a semen analysis, can help physicians create a more personalized and effective treatment plan for couples trying to conceive. For example, our studies have shown that those with Poor sperm quality have a 3x lower chance of successful pregnancy when undergoing IUI, but that IVF is still likely to work. What’s more, we found that 4 out of 5 men who received a Poor result based on the sperm epigenetic profile showed “normal” semen parameters otherwise–meaning they may not have been considering male factors.
Path SpermQT is a physician-ordered test. Learn more about how to get your sperm tested with Path SpermQT.
Advanced Sperm Quality Testing. Easy, Mail-in Kit.
Learn More9. Treatment of Male Infertility
The goal of fertility treatment is conception, pregnancy, and the birth of your child. If surgical approaches such as varicocele repair are not able to address the cause of infertility, additional therapies may be used. Intrauterine insemination (IUI) involves washing ejaculated sperm and introducing the specimen into the cervix with a special pipette during a modified gynecological exam. In cases of very low or absent ejaculated sperm counts, sperm are typically collected from the ejaculate or through surgical testicular extraction and introduced to the egg through assisted reproduction therapies such in-vitro fertilization (IVF), or injected directly into the egg (IVF-ICSI). Success rates vary for each technique, but IVF and IVF-ICSI are statistically more successful than IUI. Financial costs for each procedure vary, though IVF and IVF-ICSI may cost up to 10X more than IUI.
10. Approaching Infertility & Treatment
Coping with infertility can be difficult and the journey through treatment can be long and stressful. Specifically, it’s an issue of the unknown–you can’t predict how long treatment will take and what the outcome will be. The emotional burden on a couple is considerable. Talking with your partner about expectations and putting together a mutually agreed upon plan can help weather the process. Decide in advance how many and what kind of procedures are emotionally and financially acceptable for you and your partner and determine a final limit.