Failed IVF cycles can be emotionally painful, not to mention costly. However, that doesn’t mean that couples should give up. There is strong evidence suggesting that undergoing multiple rounds of IVF will increase your chances of getting pregnant.
The Increasing Use of IVF
In vitro fertilization (IVF) is a type of assisted reproductive technology (ART). Eggs are retrieved from ovaries, sperm is collected from a semen sample, and the sperm fertilizes the egg in a lab. Then, the fertilized eggs (known as embryos) are transferred to a uterus and hopefully result in a successful pregnancy.
IVF is an increasingly more common way for couples to conceive. Between 2010 and 2019, the number of ART cycles started more than doubled in the US. Technological advances and ongoing procedural improvements are also making ART more effective. In the same time period, the number of live births resulting from ART increased by almost 70%. According to the Mayo Clinic, IVF is the most effective form of ART overall.
How many IVF cycles does it take to get pregnant?
A female’s age is the primary indicator of how successful a cycle will be. However, even women under 35 only average a 37% success rate. While it helps to remain optimistic, couples should not approach IVF as something that will guarantee a successful pregnancy on the first try.
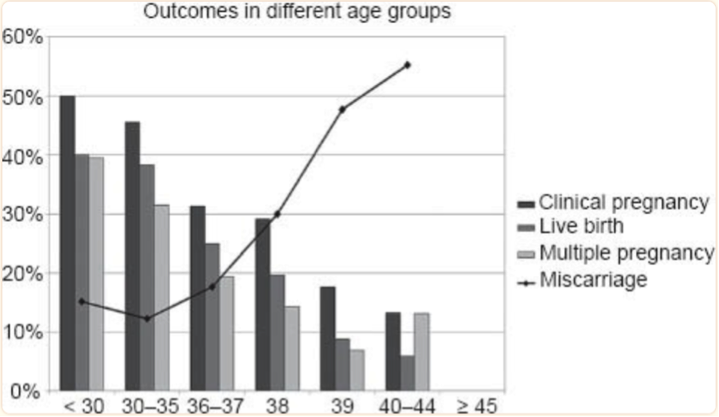
Figure Source: Tan TY, Lau SK, Loh SF, Tan HH. Female aging and reproductive outcome in assisted reproduction cycles. Singapore Med J. 2014 Jun;55(6):305-9. doi: 10.11622/smedj.2014081. PMID: 25017405; PMCID: PMC4294057.
Studies examining the likelihood of pregnancy after multiple IVF cycles show varied results. Some suggest that three rounds is the optimal number, given the emotional and financial strain that IVF can cause.
Financial limitations aside, it actually may be worth continuing beyond three IVF cycles.
One study from the UK looked at 184,269 complete cycles. It found that, on average, there was a 29% chance for a live birth after one cycle. However, the chance for a live birth went up to 43% after six complete cycles. Younger women see even higher rates of success. For example, the study shows a 30 year old woman with primary unexplained infertility has a 46% success rate in her first cycle and a 93% success rate over 6 cycles.
Generally, such studies show that the cumulative effect of trying multiple IVF rounds can lead to higher chances of pregnancy. Nevertheless, making the decision to continue or stop trying is highly personal. It should be made in consideration of all psychological, financial, and health risk factors.
What are the risks associated with IVF?
A study published in the Canadian Medical Association Journal showed a strong association between several unsuccessful rounds of IVF and cardiovascular complications. This led to a belief that IVF could cause heart disease and stroke. Researchers acknowledge that while there may be a correlation between the two, IVF does not necessarily cause cardiovascular issues. Instead, people who have underlying cardiovascular problems might have a lower chance of getting pregnant in the first place.
IVF comes with other risks such as medication and hormonal side effects, Ovarian Hyperstimulation Syndrome, and multiple births, and others. It is possible that IVF could cause additional long term health effects that have not been researched yet.
Side effects of IVF treatments have been widely documented both in medical communities and in popular culture. Female partners undergoing IVF take various medications, both oral and via injection, to stimulate the ovaries and trigger ovulation. Across such medications, side effects can potentially include hot flashes, nausea, breast tenderness, headaches, blurred vision, depression, mood swings, pelvic discomfort, decreased blood pressure, and increased incidence of miscarriage and preterm delivery.
Another considerable risk is multiple births. Women sometimes will opt for multiple embryo transfers at one time to try to increase the chances of pregnancy instead of undergoing multiple rounds of IVF. However, multiple embryo transfers can lead to multiple births (i.e. twins, triplets, etc.). In fact, the Center for Disease Control (CDC) found that 43% of babies conceived through IVF were twins. Risks associated with multiple births include preterm delivery, low birth weight, maternal complications, as well as the higher cost of neonatal and continued care.
What is Ovarian Hyperstimulation Syndrome (OHSS)?
Ovarian Hyperstimulation Syndrome (OHSS) can occur when excess hormones in the body cause the ovaries to swell and become painful. It is more common in women who are undergoing IVF with hormone injections compared to those taking oral medications for fertility treatment. Symptoms can begin within a week of starting injections and may include abdominal pain and bloating, nausea, vomiting, diarrhea, and tenderness. More severe cases can cause rapid weight gain, severe pain, persistent nausea and vomiting, blood clots, decreased urination, and shortness of breath.
How often can I do IVF treatments?
Side effects aside, many women wonder how often they should be attempting IVF or how many IVF cycles they can do safely.
It is generally standard to wait until a full menstrual cycle has passed to try another IVF cycle after a failed attempt. Some people choose to wait longer in between cycles for financial reasons, to take a break from the physical effects of medications, to recover emotionally, or for other personal considerations. The American Society for Reproductive Medicine (ASRM) found that there is no difference in pregnancy or birth rates between IVF cycles done immediately in succession or those with longer periods in between.
While there is no limit to the number of cycles you can try, it is important to keep in mind the strong effect of aging on success rates. As previously described, the older a patient gets, the lower their chances of pregnancy will be, and the cumulative psychological toll of multiple failed IVF rounds can be significant. The same reasons for taking a longer break in between cycles can also cause a couple to drop out of treatments altogether. If that is the case, there are still other options for having a child, such as surrogacy and adoption.
If my first IVF cycle fails, can I improve my chances for the next round?
It is important that your doctor investigates why the first IVF round was unsuccessful before trying a second attempt, as there are many complex variables to consider.
One source of fertility problems that is often overlooked is the male. Female age is generally accepted as the single most important factor in determining fertility, but that doesn’t mean problems on the male side can’t contribute as well. If a couple has undergone IVF, it is likely the male partner has already had a semen analysis. However, a semen analysis is a poor predictor for male fertility, and only reveals the most obvious male fertility problems.
Problems in sperm DNA can lead to poor embryo development but are more difficult to assess. If you have failed an IVF cycle, and are diagnosed with unexplained infertility, take a closer look at sperm quality. Path Fertility offers a unique, at-home sperm quality test called Path SpermQT that measures sperm cells’ ability to function properly based on epigenetic patterns within the sperm’s DNA.
Some studies also show that improving lifestyle factors can play an important role in increasing your chances of getting pregnant. Quitting smoking, cutting back on alcohol, exercising more, eating healthier, and managing stress can help to prime your body for conception–both on the male and female side.
Everyone’s path to pregnancy is different. IVF is an excellent option for conceiving a child for those who can afford the time, cost, and disruptive nature of the procedure. While chances of pregnancy do increase with multiple attempts, there are no guarantees of success. Your best option is always the one that works with your lifestyle.